Leukaemia is a form of cancer that impacts the blood and bone marrow. It originates when the DNA of a single cell within your bone marrow undergoes mutations, rendering it incapable of normal development and functioning. Leukaemia cells frequently exhibit abnormal behaviour similar to that of white blood cells.
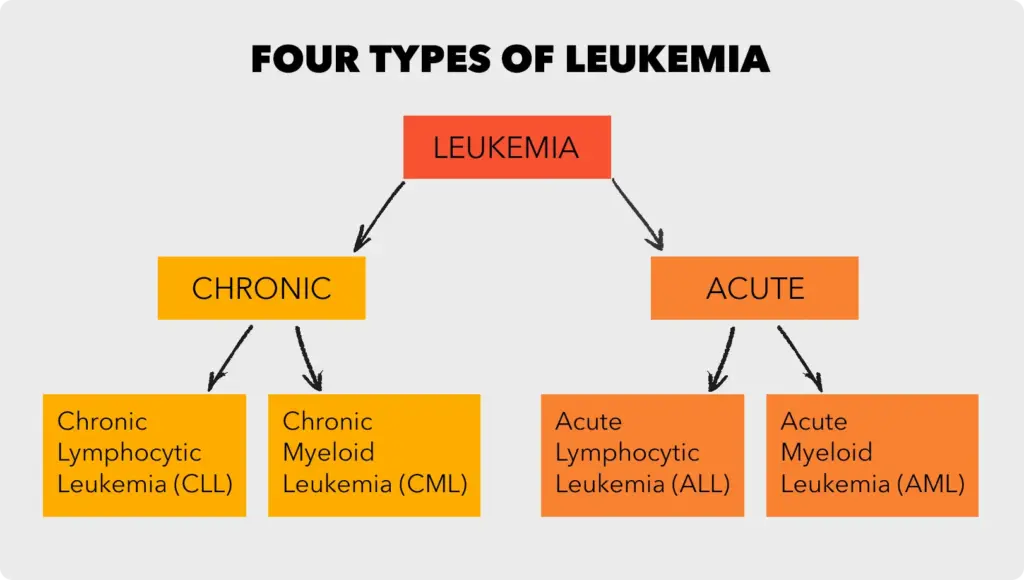
There are numerous types of leukaemia, yet they all fall into two primary categories: acute and chronic. Acute leukaemia progresses rapidly and can prove fatal without prompt intervention, while chronic leukaemia advances more gradually and may not necessitate immediate treatment.
Leukaemia Causes
The precise cause of leukaemia remains elusive, although scientists speculate that it arises from a combination of genetic and environmental factors. Certain individuals have a heightened predisposition to develop leukaemia due to their family history or specific genetic conditions. Others may develop leukaemia following exposure to particular chemicals or radiation.
Leukaemia Symptoms
Leukaemia symptoms vary depending on the leukaemia type and its stage of progression. Common symptoms encompass:
- Fatigue
- Weakness
- Fever
- Chills
- Easy bruising or bleeding
- Weight loss
- Swollen lymph nodes
- Enlarged liver or spleen
- Night sweats
- Bone pain or tenderness
Leukemia Diagnosis
To diagnose leukaemia, your physician will conduct a physical examination and inquire about your medical history and symptoms. Additionally, they may order blood tests, bone marrow transplants, and imaging studies.
Treatment of leukaemia
The treatment for leukaemia depends on the type of leukaemia you have, your age and overall health, and if leukaemia has spread to other organs or tissues. Common treatments include:
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells.
- Radiation therapy: Radiation therapy uses high-energy beams to kill cancer cells.
- Stem cell transplant: A stem cell transplant is a procedure that replaces your diseased bone marrow with healthy bone marrow from a donor.
Prognosis for leukaemia
The prognosis for leukaemia varies depending on the type of leukaemia, the stage of diagnosis, and your overall health. However, thanks to advances in treatment, many people with leukaemia now live long and healthy lives.
If you think you may have leukaemia, it is important to see a doctor right away. Early diagnosis and treatment can improve your chances of a cure.
Acute Leukemia: What You Need to Know

Acute leukaemia is a form of cancer originating in the blood-forming tissues within the bone marrow. It is characterized by the rapid proliferation of immature blood cells known as blasts. These blasts overpopulate the bone marrow, displacing healthy blood cells and resulting in a range of symptoms, including fatigue, shortness of breath, easy bruising and bleeding, and increased susceptibility to infections.
There are two primary types of acute leukaemia: acute lymphocytic leukemia (ALL) and acute myeloid leukaemia (AML). ALL is the predominant leukaemia type in children, whereas AML is most frequently diagnosed in adults.
Symptoms of Acute Leukemia
Symptoms of acute leukaemia can vary depending on the leukaemia subtype and its stage of development. Nevertheless, common symptoms encompass:
- Fatigue
- Shortness of breath
- Easy bruising and bleeding
- Increased susceptibility to infections
- Pallor (pale skin)
- Fever
- Night sweats
- Swollen lymph nodes
- Bone pain
- Headaches
- Weight loss
Causes of Acute Leukemia
Although the exact cause of acute myeloid leukaemia remains elusive, it is believed to result from a combination of genetic and environmental factors. Some risk factors include:
- Age: Acute leukaemia is more prevalent in both children and older adults.
- Family history: A family history of leukaemia elevates the risk.
- Genetic disorders: Certain genetic conditions, such as Down syndrome and Klinefelter syndrome, can increase susceptibility to leukaemia.
- Exposure to radiation or specific chemicals: High levels of radiation or exposure to certain chemicals like benzene can heighten the risk of developing leukaemia.
Diagnosis of Acute Leukemia
The diagnosis of acute leukaemia relies on a physical examination, medical history, and blood tests. Blood tests can reveal the presence of blasts in the blood. Additionally, a bone marrow biopsy may be performed to confirm the diagnosis and determine the specific leukaemia subtype.
Treatment of Acute Leukemia
Treatment for acute leukaemia hinges on factors like the leukaemia subtype, disease stage, and the patient’s age and overall health. Common treatment options comprise:
- Chemotherapy: The use of drugs to target and eradicate cancer cells.
- Radiation therapy: The application of high-energy radiation to eliminate cancer cells.
- Stem cell transplant: A procedure involving the replacement of a patient’s bone marrow with healthy stem cells from a donor.
Prognosis for Acute Leukemia
The prognosis for acute leukaemia has notably improved in recent years. Currently, more than 80% of children diagnosed with ALL can be cured. While the prognosis for AML is not as favourable, it has also shown improvement. The 5-year survival rate for adults with AML now stands at approximately 25%.
Ongoing Research on Acute Leukemia
Ongoing research aims to advance our understanding of acute leukaemia and develop more effective treatments. Areas of research include:
- Targeted therapy: Utilizing drugs that specifically target molecules involved in leukaemia cell growth and survival.
- Immunotherapy: Enhancing the body’s immune system to combat cancer cells.
- Gene therapy: Modifying or replacing defective genes within cancer cells to halt their growth or eliminate them.
If you have any concerns about acute leukaemia, it is advisable to consult with your physician.
Chronic leukaemia: Symptoms, diagnosis, and treatment

Chronic leukaemia is a form of cancer originating in the body’s blood-forming tissues, including the bone marrow. In this condition, the cancer cells consist of immature white blood cells that grow slowly and gradually replace healthy blood cells.
There are two primary types of chronic leukaemia:
- Chronic lymphocytic leukaemia (CLL): This is the most prevalent type of leukaemia in adults, commencing in lymphocytes, a specific type of white blood cell that plays a crucial role in infection defence.
- Chronic myeloid leukemia (CML): CML initiates in myeloid cells, which are immature white blood cells capable of developing into various blood cell types.
Additional types of chronic leukaemia encompass hairy cell leukemia, chronic myelomonocytic leukaemia, and chronic eosinophilic leukaemia.
Symptoms of Chronic Leukemia
Initially, many individuals with chronic leukaemia exhibit no symptoms. Signs and symptoms may manifest as the cancer progresses, and they might include:
- Enlarged lymph nodes
- Fatigue
- Fever
- Upper left abdominal pain
- Night sweats
- Weight loss
- Frequent infections
Diagnosis of Chronic Leukemia
Chronic leukaemia is frequently detected through routine blood tests. Elevated white blood cell counts or abnormal white blood cells in a blood test may prompt further assessments, including a bone marrow biopsy.
Treatment for Chronic Leukemia
The treatment of chronic leukaemia hinges on factors such as the leukaemia subtype, disease stage, and the patient’s overall health. Some individuals with chronic leukaemia may not require immediate treatment, while others may necessitate intervention to manage the disease and avert complications.
Common treatments for chronic leukaemia encompass:
- Chemotherapy: Employing chemotherapy drugs to eliminate cancer cells
- Targeted therapy: Using targeted therapy drugs to specifically target molecules involved in cancer cell growth and survival
- Immunotherapy: Administering immunotherapy drugs to bolster the body’s immune system to combat cancer cells.
- Stem cell transplantation: A procedure involving the replacement of diseased bone marrow with healthy stem cells.
Prognosis of Chronic Leukemia
The prognosis for individuals with chronic leukaemia varies based on the leukaemia type and the disease’s stage at diagnosis. Some people with chronic leukaemia can live for many years with the condition, while others may require multiple treatments or may eventually succumb to the disease.
Research on Chronic Leukemia
Researchers are diligently working on developing novel and more effective treatments for chronic leukaemia. Additionally, they are striving to identify the causes of chronic leukaemia with the aim of prevention.
If you possess any inquiries or concerns regarding chronic leukaemia, it is advisable to consult with your physician.
Rare Blood Cancers: A Serious but Treatable Group of Diseases

Rare blood cancers encompass a group of malignancies that impact blood cells, bone marrow, or the lymphatic system. They are less prevalent compared to more common blood cancers like leukaemia, lymphoma, and myeloma; nonetheless, they can pose significant threats to one’s health and life.
Numerous types of rare blood cancers exist, with some of the most frequently encountered ones being:
Myeloproliferative neoplasms (MPNs):
MPNs are a category of rare blood cancers arising when the body excessively produces white blood cells, red blood cells, or platelets. The principal MPN subtypes comprise:
- Essential thrombocythemia (ET): ET results in an excessive production of platelets, which are crucial for clot formation and preventing bleeding.
- Polycythemia vera (PV): PV leads to an overproduction of red blood cells, responsible for oxygen transport to the body’s tissues.
- Myelofibrosis (MF): MF causes the bone marrow to become fibrous and scarred, hindering the production of healthy blood cells.
Histiocytosis:
Histiocytosis refers to a cluster of rare blood disorders that trigger an overproduction of histiocytes, a type of white blood cell involved in infection and inflammation control. Various histiocytosis subtypes include Langerhans cell histiocytosis (LCH), Erdheim-Chester disease (ECD), and Rosai-Dorfman disease (RDD).
Paroxysmal nocturnal hemoglobinuria (PNH):
PNH is an uncommon blood disorder leading to the body’s destruction of its red blood cells, culminating in anaemia, fatigue, and breathlessness.
Diagnosing rare blood cancers can be challenging due to their potential to mimic other medical conditions. Symptoms can diverge depending on the specific cancer type, but some prevalent indicators include:
- Fatigue
- Weakness
- Shortness of breath
- Pallor
- Easy bruising or bleeding
- Bone pain
- Night sweats
- Fever
- Unexplained weight loss
If you experience any of these symptoms, seeking medical evaluation is crucial for a timely diagnosis.
Treatment for rare blood cancers fluctuates depending on the cancer type and its stage. Common treatment options encompass chemotherapy, radiation therapy, and stem cell transplantation.
While treating rare blood cancers can be complex, substantial progress has been made in recent years. Thanks to innovative and novel therapies, many individuals with rare blood cancers can now lead long and productive lives.
If you or someone you know is dealing with a rare blood cancer diagnosis, it is vital to access support from healthcare professionals and others who have faced similar challenges. Numerous resources are available, including support groups, patient advocacy organizations, and financial assistance programs.
Leukaemia in Children

Leukaemia is a cancer of the blood cells. It starts in the bone marrow, where new blood cells are made. Leukaemia cells crowd out healthy blood cells, making it difficult for the body to fight infection, prevent excessive bleeding, and carry oxygen throughout the different parts of the body.
Leukaemia is the most common cancer in children and teens, accounting for almost 1 out of 3 cancers. Most childhood leukaemias are acute, meaning they progress rapidly. Chronic leukaemias are less common in children and develop more slowly.
Types of Leukemia in Children
The three main types of leukaemia in children are:
- Acute lymphoblastic leukemia (ALL): ALL is the most common type of childhood leukaemia, accounting for about 85% of cases. It impacts lymphocytes, a category of white blood cells.
- Acute myeloid leukemia (AML): AML is the second most frequent childhood leukaemia, making up about 15% of cases. It affects myeloid cells, which possess the capability to develop into various blood cell types, including red blood cells, white blood cells, and platelets.
- Chronic myelogenous leukaemia (CML): CML is an infrequent childhood leukaemia, comprising less than 1% of cases. It originates in myeloid cells but progresses more slowly than AML.
Symptoms of leukaemia in children
Symptoms of leukaemia in children vary contingent on the leukaemia type and its stage of advancement. Common symptoms encompass:
- Fatigue
- Pallor
- Easy bruising or bleeding
- Frequent infections
- Fever
- Shortness of breath
- Swollen lymph nodes
- Abdominal discomfort
- Bone or joint pain
- Headaches
Should you observe any of these symptoms in your child, immediate consultation with a doctor is crucial.
Treatment for leukaemia in children
The treatment for childhood leukaemia depends on factors like the leukaemia subtype, the child’s age and overall health, and the stage of leukaemia. Typical treatment approaches encompass:
- Chemotherapy: Utilizing chemotherapy drugs to eradicate cancer cells.
- Radiation therapy: Employing high-energy radiation to eliminate cancer cells.
- Stem cell transplant: A procedure in which the child’s bone marrow is replaced with healthy stem cells.
The prognosis for leukaemia in children
The prognosis for childhood leukaemia has substantially improved over the past decades. Presently, more than 90% of children with ALL achieve a cure. The prognosis for children with AML is also promising, with approximately 70% of children experiencing a cure. However, the prognosis for children with CML is less favourable, with approximately 50% achieving a cure.
Research on leukaemia in children
Ongoing research in childhood leukaemia is exploring innovative and improved treatments. Some encouraging areas of research include:
- Targeted therapy: Targeted therapy drugs designed to specifically target molecules on cancer cells.
- Immunotherapy: Immunotherapy strategies to bolster the body’s immune system in combating cancer cells.
- Gene therapy: Experimental treatments involving the alteration of cancer cell genes to enhance their susceptibility to treatment.
If your child or someone you know has received a leukaemia diagnosis, it is crucial to engage in discussions with your doctor regarding the latest research findings and available treatment options
Targeted therapy for leukaemia: A more precise approach

Targeted therapy represents a distinctive approach to treating cancer, characterized by the use of drugs or specific substances to pinpoint and combat cancer cells. Unlike conventional chemotherapy, which indiscriminately affects both cancerous and healthy cells, targeted therapies focus on disrupting the precise molecules that facilitate the growth and survival of cancer cells.
Targeted therapy is a viable option for addressing various forms of leukaemia, including acute lymphoblastic leukaemia (ALL), acute myeloid leukaemia (AML), and chronic lymphocytic leukemia (CLL). It is often administered in conjunction with other cancer treatments such as chemotherapy and radiation therapy.
Targeted therapy for leukaemia
Numerous types of targeted therapy drugs are available for leukaemia treatment, with some of the most prevalent categories including:
- Tyrosine kinase inhibitors (TKIs): TKIs are drugs designed to inhibit tyrosine kinases, enzymes crucial for cell growth and division. They are particularly effective in treating ALL and CLL cases with specific genetic mutations.
- Monoclonal antibodies: Monoclonal antibodies are synthetic proteins created in laboratories, capable of binding to specific molecules found on cancer cells. This binding can either directly eliminate cancer cells or facilitate the delivery of other drugs, like chemotherapy, to the cancer cells.
- BCR-ABL inhibitors: These targeted therapy drugs are employed in the treatment of chronic myeloid leukaemia (CML). CML results from a genetic mutation that generates a fusion protein called BCR-ABL. BCR-ABL inhibitors obstruct the activity of this fusion protein, impeding the growth and spread of leukaemia cells.
It’s crucial to note that while targeted therapy can be highly effective in treating leukaemia, it may not serve as a cure for all patients. Some individuals may develop resistance to these drugs over time, while others may experience side effects during treatment.
Nonetheless, targeted therapy has brought about a transformative shift in leukaemia treatment in recent years, enhancing survival rates and the overall quality of life for numerous patients.
Benefits of targeted therapy for leukaemia:
- Precision: Targeted therapies are designed to selectively target molecules on cancer cells, minimizing harm to healthy cells.
- Enhanced effectiveness: Targeted therapies can be more potent at eliminating cancer cells, particularly in cases with specific genetic mutations.
- Fewer side effects: Targeted therapies often lead to fewer side effects compared to traditional chemotherapy, as they are less likely to harm healthy cells.
Side effects of targeted therapy for leukaemia
Side effects associated with targeted therapy for leukaemia may vary based on the specific drug utilized. However, some common side effects encompass:
- Fatigue
- Nausea and vomiting
- Diarrhea
- Hair loss
- Skin rash
- Anemia
- Thrombocytopenia
- Neutropenia
If you are contemplating targeted therapy as a leukaemia treatment option, it is imperative to engage in a comprehensive discussion with your physician regarding potential risks and benefits.
Leukaemia treatment duration varies

The duration of leukaemia treatment can vary based on leukaemia type, patient age, and other factors. Generally, leukaemia treatment spans from several months to several years.
The most prevalent form of treatment for leukaemia is chemotherapy. Chemotherapy drugs target cancer cells but can also harm healthy cells, leading to side effects like hair loss, nausea, and vomiting. Typically, chemotherapy is administered in cycles, each spanning several weeks. The number of cycles required depends on the leukemia type and patient response.
Radiation therapy might be necessary in certain cases. This treatment employs high-energy rays to eliminate cancer cells, usually administered daily over several weeks.
If chemotherapy and radiation therapy prove ineffective, or if leukaemia recurs, a stem cell transplant may be needed. This procedure replaces a patient’s bone marrow with healthy marrow from a donor. Although effective, stem cell transplants are high-risk.
Breakdown of typical leukaemia treatment duration
Here’s an overview of typical leukaemia treatment durations for various types:
- Acute lymphocytic leukaemia (ALL): Predominant in children, ALL treatment lasts around two to three years.
- Acute myeloid leukaemia (AML): Common in adults, AML treatment spans four to six months.
- Chronic lymphocytic leukaemia (CLL): Slow-growing leukaemia, CLL may not need immediate treatment but, when initiated, typically persists for life.
- Chronic myeloid leukaemia (CML): Another slow-growing type, CML treatment is usually lifelong but manageable with targeted therapy drugs.
These are general guidelines, and individual treatment duration varies.
How can you cope with the long duration of leukaemia treatment?
Consider these strategies for coping with the lengthy leukaemia treatment:
- Assemble a robust support network. Family and friends offer invaluable support during treatment; communicate your feelings and needs to them.
- Seek out a support group. Numerous support groups cater to leukaemia patients and their families, providing a valuable community of understanding peers.
- Take periodic treatment breaks. When possible, pause treatment to spend time with loved ones, pursue hobbies, or relax. These breaks can foster positivity and motivation.
- Prioritize health. Focus on maintaining your physical and mental well-being during treatment through a nutritious diet, sufficient sleep, and regular exercise.
- Remember, you’re not alone. Many people care about your journey and are willing to support you through it.














